Print this page • Back to Web version of article
“Deep salvage patients no longer exist. The ones in that situation are already dead or have responded to the latest HIV antiretrovirals.”
“Even if we give expanded access to multiple investigational agents to patients in salvage therapy, it will be a waste since most of these patients have adherence problems.”
“It is too expensive and cumbersome for my clinic to provide expanded access.”
“My institution no longer participates in expanded access due to costs and manpower problems.”
These are statements that I have heard in different meetings that I have attended in the recent past to discuss access and research issues in HIV. Some of these statements are very hard for me to hear, since I am one of these “difficult patients” who have “failed” most commercially available medications — despite the fact that I, like many of my peers, am certainly not a patient who lacks perfect adherence.
Most of us built resistance as we joined study after study that exposed us to functional monotherapy. In fact, I consider many of us who have been struggling with multiple drug resistance to be wounded soldiers from a time when we were recruited into studies we joined out of desperation to access a new drug. Even if we seem invisible due to our lower numbers, we are still here — and we absolutely hate to be discounted as disposable in the current era of largely successful HIV treatment.
It is my opinion, and that of several clinicians that I have worked with, that it is the pharmaceutical industry’s duty to provide access to multiple investigational drugs so that so-called “salvage patients,” such as myself, can finally construct a regimen that may help us join the population of virologically controlled patients.
We all know that the management of resistant HIV disease has improved dramatically with the approval of a number of highly effective antiretroviral drugs, including darunavir (TMC114, Prezista), etravirine (TMC125, Intelence), maraviroc (Selzentry, Celsentri) and raltegravir (Isentress). Among this recent generation of antiretroviral drugs, perhaps the most promising is raltegravir, the first clinically available inhibitor of HIV integrase. When used in combination with other active drugs, raltegravir has proven to be very potent, well tolerated and highly effective. In phase 2 and 3 clinical trials, the vast majority of patients who were able to combine raltegravir with at least one other active drug achieved durable viral suppression. (Comparable efficacy has been seen in patients who received darunavir, etravirine or maraviroc with at least one other effective agent.)
Despite the impressive effectiveness of these drugs in clinical trials, a subset of patients has exhibited virologic failure while on these drugs. Most failures likely occurred because of the inability to construct a regimen that contained two to three fully effective agents. Adverse events, drug-drug interactions and non-adherence also likely contributed to the inability of some patients on these drugs to achieve durable viral suppression. As a consequence of these factors, the failure rates in the recent phase 3 studies — DUET (etravirine and darunavir), MOTIVATE (maraviroc) and BENCHMRK (raltegravir) — were in the 27% to 40% range.
The picture gets less encouraging when looking at longer-term data. As shown in the following figure, a longer-term study generated from following patients using raltegravir for 144 weeks showed failure rates of 40% to 56% even in patients with one or more active agents in their background therapy.
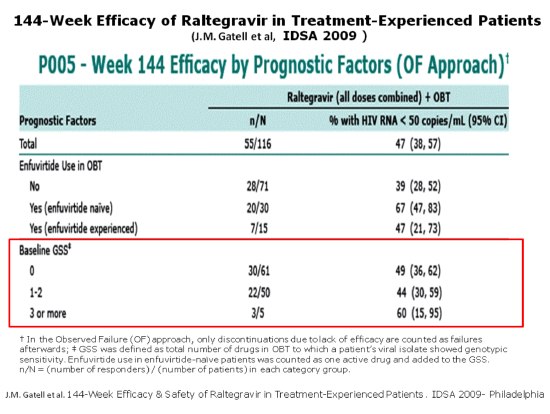 |
But I guess these patients disappear into the dark, since many physicians do not seem to know who they are. It is assumed that many of the patients who failed these recent studies were subsequently unable to construct a suppressive regimen, although the long-term outcomes of those failing these clinical trials are unknown.
The prevalence of multi-regimen failure in clinical practice is also unknown. Steven Deeks, M.D., and colleagues at the University of California San Francisco/San Francisco General Hospital have an ongoing observational cohort of patients who have developed drug-resistant HIV (the SCOPE cohort). Most of these patients have been able to construct a fully suppressive regimen and are currently doing well clinically.
However, of the original 300 SCOPE patients, approximately 40 now have evidence of having failed all six therapeutic drug classes. These 40 patients have a genotypic sensitivity score (GSS) of either zero or one, and they have no clear options for suppressing HIV replication. Many have advanced disease (with a CD4+ cell count of less than 100 cells/mm3) and hence may not be able to “wait” for the development and approval of multiple new options.
In an informal online survey I made with the help of a team of investigators and activists, which was presented in a meeting with the U.S. Food and Drug Administration (FDA), 83 physicians around the country reported having a total of 252 patients with a GSS of zero or one.
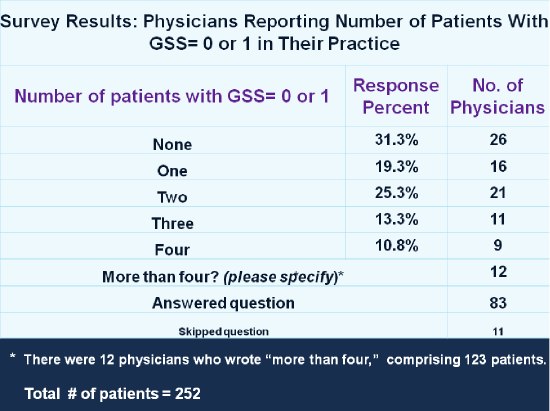 |
The most surprising finding was the wide geographical distribution of these patients. Physicians from 47 U.S. cities and towns reported treating them. Although the larger cities had the most patients with a low GSS, many patients lived in small towns that are far from research sites or large practices that are more equipped to handle the needed paperwork to apply for expanded access or single-patient emergency drug access programs.
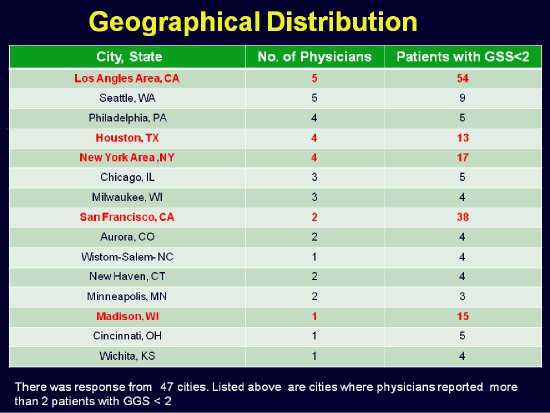 |
Much of the expanded access program documentation and nurse/physician time is not reimbursable or paid for by studies, so most doctors participating in these programs are doing so from the goodness of their hearts. Many large medical schools and clinics have stopped providing expanded access help to their patients entirely.
The following chart outlines some of the reasons reported by survey participants for not applying for early access to investigational drugs for their patients. The most common reason was that they simply did not have the administrative support they needed to handle the required paperwork. Many also expressed frustration with an application process they felt was too complex.
 |
Given that patients who are unable to construct a background regimen often fail therapy, the FDA and other interested groups have advocated that future clinical trials only enroll patients whose background regimen has a GSS or phenotypic susceptibility score greater than or equal to one. Although this is an ethically sound recommendation, one unfortunate consequence is that those patients who have now progressed to multi-regimen failure won’t be able to access experimental drugs via clinical trials.
Unfortunately, the HIV drug pipeline in 2011 is a lot more limited than it has been in the past due to many factors, including the relatively small size of the U.S. market, drug development costs, and the difficulty in finding treatment-experienced patients with one or more active agents in their background therapy. Some drugs have already been abandoned due to these issues, as shown by this table.
 |
Thankfully, the FDA has proposed a new trial design concept that will facilitate the development of medications for treatment-experienced patients, which may encourage pharmaceutical companies not to abandon HIV drug development. For more information about this novel trial design concept, refer to a presentation given by Jeffrey Murray, M.D., M.P.H., from the FDA at a recent meeting sponsored by the Forum for Collaborative HIV Research.
However, even with these efforts, the possibility of constructing a regimen with three active agents for the salvage population within the next four years is low, which will diminish the chances for survival in those with lower CD4+ cell counts.
I’ve laid out a grim scenario in this blog post, but in my next post, I’ll discuss a potential silver lining: a program in the works that I hope will greatly expand options for deep salvage patients in need of access to investigational agents.
This article was provided by The Body PRO. You can find this article online by typing this address into your Web browser:
https://www.thebodypro.com/content/art61780.html