| From the book: Built to Survive
12.
Complementary Approaches to Treating Lipodystrophy |
By
Michael Mooney
(original version in
Medibolics 2(2),Nov. 1997)
|
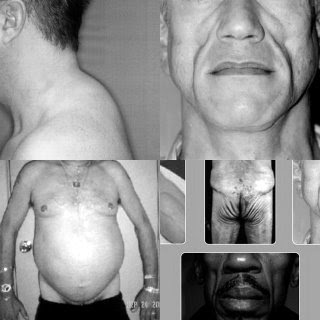
While
the protease inhibitor (PI) cocktails can bring viral loads down to
undetectable levels and have given many HIV(+) people a new lease on life,
protease inhibitors are not always benign drugs. As we approach year four of
the triple-combo era, numerous problems have appeared among people who are on
protease inhibitors. One of the most common of these side effects (and perhaps
the least understood) is the protease belly or Crix belly phenomenon. Crix belly, so named because it
was mostly observed among people being treated with Crixivan, is a condition most notably
marked by the appearance of a large protruding potbelly. (At the same time this
is happening some people report that they feel like they are losing muscle mass
and fat, too, especially in the arms and legs.) Another sometimes concurrent
but rare condition is the so-called buffalo hump, which is a fat pad that
grows on the back of the neck that resembles what is seen in Cushing’s syndrome. Women are also experiencing
an increase in breast size as the breasts seem to gain fat (called lipoma), and many people are losing
fat in their arms, legs, and cheeks while one or more of these other things are
happening to them. Lipodystrophy is the medical term that has been given to
this syndrome, but it can also simply be called bodyfat redistribution.
the protease inhibitor (PI) cocktails can bring viral loads down to
undetectable levels and have given many HIV(+) people a new lease on life,
protease inhibitors are not always benign drugs. As we approach year four of
the triple-combo era, numerous problems have appeared among people who are on
protease inhibitors. One of the most common of these side effects (and perhaps
the least understood) is the protease belly or Crix belly phenomenon. Crix belly, so named because it
was mostly observed among people being treated with Crixivan, is a condition most notably
marked by the appearance of a large protruding potbelly. (At the same time this
is happening some people report that they feel like they are losing muscle mass
and fat, too, especially in the arms and legs.) Another sometimes concurrent
but rare condition is the so-called buffalo hump, which is a fat pad that
grows on the back of the neck that resembles what is seen in Cushing’s syndrome. Women are also experiencing
an increase in breast size as the breasts seem to gain fat (called lipoma), and many people are losing
fat in their arms, legs, and cheeks while one or more of these other things are
happening to them. Lipodystrophy is the medical term that has been given to
this syndrome, but it can also simply be called bodyfat redistribution.
It
now appears that lipodystrophy is not a side effect entirely specific to
Crixivan. It may be seen with use of any of the available
protease inhibitors, and nucleoside and non-nucleoside analogs. It has also
been seen to a lesser degree in HIV(+) people before protease inhibitors were
available. However, the various cocktails of powerful drugs being used today to
combat HIV seem to increase the severity of this syndrome over the simpler drug
combos of a few years ago, although there is discussion that one of the older
drugs, D4T (Zerit) may play a central role in the problem (visit https://www.facialwasting.org/
pages/891053/index.htm ) . And in some cases, the addition of the appetite
stimulant Megace to the protease inhibitors seems to increase
the potential for bodyfat redistribution.
now appears that lipodystrophy is not a side effect entirely specific to
Crixivan. It may be seen with use of any of the available
protease inhibitors, and nucleoside and non-nucleoside analogs. It has also
been seen to a lesser degree in HIV(+) people before protease inhibitors were
available. However, the various cocktails of powerful drugs being used today to
combat HIV seem to increase the severity of this syndrome over the simpler drug
combos of a few years ago, although there is discussion that one of the older
drugs, D4T (Zerit) may play a central role in the problem (visit https://www.facialwasting.org/
pages/891053/index.htm ) . And in some cases, the addition of the appetite
stimulant Megace to the protease inhibitors seems to increase
the potential for bodyfat redistribution.
There
are several reasons why this might happen. The “protease pouch belly” in many
respects resembles the potbelly seen in disease states like Cushing’s syndrome, alcoholic hepatitis, and heart disease. In these
diseases the potbelly is associated with the development of insulin resistance [i] [ii] [iii] and is primarily composed of enlarged fat
deposits surrounding the visceral organs, like the stomach, and liver, under
the abdominal muscle wall and ribs.[iv] The potential for liver burden or
toxicity induced by many of the common AIDS medications has been documented and
the protease inhibitors are no exception to this rule. Elevated triglycerides,
liver enzymes, and blood glucose and even diabetes have all been observed in patients on protease
inhibitor therapy. All of these conditions are symptoms
of diminished insulin sensitivity, and we are seeing that the protease
inhibitors’ effects on liver metabolism are inducing a state of insulin
resistance in many people who are on protease inhibitor
therapy. Complications of insulin resistance include hyperglycemia (high blood sugar), diabetes, and
cardiovascular disease, and the FDA has documented over 80 cases of diabetes
that appear to be associated with protease inhibitor therapy.
are several reasons why this might happen. The “protease pouch belly” in many
respects resembles the potbelly seen in disease states like Cushing’s syndrome, alcoholic hepatitis, and heart disease. In these
diseases the potbelly is associated with the development of insulin resistance [i] [ii] [iii] and is primarily composed of enlarged fat
deposits surrounding the visceral organs, like the stomach, and liver, under
the abdominal muscle wall and ribs.[iv] The potential for liver burden or
toxicity induced by many of the common AIDS medications has been documented and
the protease inhibitors are no exception to this rule. Elevated triglycerides,
liver enzymes, and blood glucose and even diabetes have all been observed in patients on protease
inhibitor therapy. All of these conditions are symptoms
of diminished insulin sensitivity, and we are seeing that the protease
inhibitors’ effects on liver metabolism are inducing a state of insulin
resistance in many people who are on protease inhibitor
therapy. Complications of insulin resistance include hyperglycemia (high blood sugar), diabetes, and
cardiovascular disease, and the FDA has documented over 80 cases of diabetes
that appear to be associated with protease inhibitor therapy.
Indeed,
from early 1998, numerous studies have documented an association between the
use of protease inhibitors and measurements that indicate insulin resistance is present including data by
Kathleen Mulligan, Ph.D. of San Francisco
General Hospital, confirming that protease inhibitors can cause the blood
chemistry changes that are typical of insulin resistance;[v]
Dr. Ravi Walli of
Ludwig-Maximilians Universitat Munchen in Germany reporting that peripheral
insulin resistance is common in patients on protease inhibitors;[vi]
and Dr. Andrew Carr of St.
Vincent’s Hospital of Sydney, Australia, detailing his hypothesis of the
cytoplasmic (cellular) retinoic acid-binding protein type I (CRABP-1)
biochemistry involved in the liver dysfunction that may promote insulin
resistance.[vii]
Additionally, some people who are using protease inhibitors are being found to
have accelerated cardiovascular disease, which is also a common outcome of
progressive insulin resistance.
from early 1998, numerous studies have documented an association between the
use of protease inhibitors and measurements that indicate insulin resistance is present including data by
Kathleen Mulligan, Ph.D. of San Francisco
General Hospital, confirming that protease inhibitors can cause the blood
chemistry changes that are typical of insulin resistance;[v]
Dr. Ravi Walli of
Ludwig-Maximilians Universitat Munchen in Germany reporting that peripheral
insulin resistance is common in patients on protease inhibitors;[vi]
and Dr. Andrew Carr of St.
Vincent’s Hospital of Sydney, Australia, detailing his hypothesis of the
cytoplasmic (cellular) retinoic acid-binding protein type I (CRABP-1)
biochemistry involved in the liver dysfunction that may promote insulin
resistance.[vii]
Additionally, some people who are using protease inhibitors are being found to
have accelerated cardiovascular disease, which is also a common outcome of
progressive insulin resistance.
A
look at Harrison’s Principles of Internal Medicine shows us that lipodystrophy
can be associated with insulin resistance, and so we see that the components
in this puzzle, lipodystrophy; elevated triglycerides, elevated blood glucose, elevated insulin levels;
diabetes; cardiovascular disease; and insulin resistance are all appearing.
look at Harrison’s Principles of Internal Medicine shows us that lipodystrophy
can be associated with insulin resistance, and so we see that the components
in this puzzle, lipodystrophy; elevated triglycerides, elevated blood glucose, elevated insulin levels;
diabetes; cardiovascular disease; and insulin resistance are all appearing.
While
this chapter does not offer a cure for body fat redistribution as protease
belly, buffalo hump, loss of facial fat, or lipoma, it offers tools that are
documented to improve insulin sensitivity that may help people gain some
control over this problem until medical science gains enough of an
understanding to solve it.
this chapter does not offer a cure for body fat redistribution as protease
belly, buffalo hump, loss of facial fat, or lipoma, it offers tools that are
documented to improve insulin sensitivity that may help people gain some
control over this problem until medical science gains enough of an
understanding to solve it.
Women and Testosterone
Studies
show that HIV(+) women who are losing lean body mass may also need testosterone, 89 but the appropriate dosage of testosterone
enanthate injections for women is usually much lower than the dosage for men,
between 2.5 and 20 mg per week. This is something for a doctor to determine by
taking blood tests, usually two to three days after the fourth weekly injection
for a representative average level. A number of HIV(+) women are using
testosterone creams that are compounded by a pharmacy like Women’s
International Pharmacy (1-800-279-5708). However, testosterone enanthate injections
deliver a longer-lasting blood level of testosterone than the creams, which
have a relatively short life span in the body. If a cream is used, it is
usually applied in a dose of between 2 and 5 mg two times per day, while the
injections are best given once per week, as studies show that testosterone
blood levels generally decline to baseline within about 10 days after
injection.[xix]
show that HIV(+) women who are losing lean body mass may also need testosterone, 89 but the appropriate dosage of testosterone
enanthate injections for women is usually much lower than the dosage for men,
between 2.5 and 20 mg per week. This is something for a doctor to determine by
taking blood tests, usually two to three days after the fourth weekly injection
for a representative average level. A number of HIV(+) women are using
testosterone creams that are compounded by a pharmacy like Women’s
International Pharmacy (1-800-279-5708). However, testosterone enanthate injections
deliver a longer-lasting blood level of testosterone than the creams, which
have a relatively short life span in the body. If a cream is used, it is
usually applied in a dose of between 2 and 5 mg two times per day, while the
injections are best given once per week, as studies show that testosterone
blood levels generally decline to baseline within about 10 days after
injection.[xix]
As
women are much more sensitive to side effects from testosterone, the physician should monitor
a female closely for any virilizing side effects, which include oily skin, acne, peach fuzz, hair loss, and clitoral enlargement,
and immediately lower the dose or cease the therapy if these kinds of symptoms
start to occur.
women are much more sensitive to side effects from testosterone, the physician should monitor
a female closely for any virilizing side effects, which include oily skin, acne, peach fuzz, hair loss, and clitoral enlargement,
and immediately lower the dose or cease the therapy if these kinds of symptoms
start to occur.
Normal Testosterone Levels May Not Be Enough (Men Only)
I
should also note that finding the correct testosterone dose for each individual is not always easy,
as data from studies by researchers like Dr. Judith Rabkin suggest that being HIV(+) can mean that the
normal range for testosterone measurements does not necessarily apply to men.
In her study with HIV(+) hypogonadal men, Dr. Rabkin found that the dose of
testosterone enanthate needed to be above 200 mg every two weeks, for good
quality-of-life. The dosage she found to be effective was 400 mg every two
weeks (which I suggest is best given as 200 mg per week for more consistent
blood levels, less peak/trough effect, and reduced potential for side effects).
At 400 mg given every two weeks the men’s blood testosterone levels averaged
about 1100 ng/dL one week after the fourth injection (on a scale where the
normal range is 300 to 990 ng/dL). In private correspondence Dr. Rabkin said
that she is not sure whether 300 mg every two weeks would yield a satisfactory
result or whether the men would respond satisfactorily if their average levels
only reached 800 ng/dL. She said that some men did receive benefit at about 700
ng/dL though.[xx]
Remember, the bottom of the normal scale was 300, so the normal scale didn’t
seem to apply well to these HIV(+) men.
should also note that finding the correct testosterone dose for each individual is not always easy,
as data from studies by researchers like Dr. Judith Rabkin suggest that being HIV(+) can mean that the
normal range for testosterone measurements does not necessarily apply to men.
In her study with HIV(+) hypogonadal men, Dr. Rabkin found that the dose of
testosterone enanthate needed to be above 200 mg every two weeks, for good
quality-of-life. The dosage she found to be effective was 400 mg every two
weeks (which I suggest is best given as 200 mg per week for more consistent
blood levels, less peak/trough effect, and reduced potential for side effects).
At 400 mg given every two weeks the men’s blood testosterone levels averaged
about 1100 ng/dL one week after the fourth injection (on a scale where the
normal range is 300 to 990 ng/dL). In private correspondence Dr. Rabkin said
that she is not sure whether 300 mg every two weeks would yield a satisfactory
result or whether the men would respond satisfactorily if their average levels
only reached 800 ng/dL. She said that some men did receive benefit at about 700
ng/dL though.[xx]
Remember, the bottom of the normal scale was 300, so the normal scale didn’t
seem to apply well to these HIV(+) men.
Free Testosterone
We
assert that some men’s apparent need for testosterone at higher than the standard replacement dose
of 100 mg per week (for HIV-negative hypogonadal men) may be the result of hormonal resistance
to testosterone. Hormonal resistance appears to happen with several hormones in
HIV pathology. However, studies suggest that the need for higher testosterone
doses is most likely caused by elevated sex-hormone binding globulins and
lowered free testosterone,
which is common in HIV.88 [xxi]
When this is the case, total testosterone measurements do not adequately
reflect the person’s state of health.
assert that some men’s apparent need for testosterone at higher than the standard replacement dose
of 100 mg per week (for HIV-negative hypogonadal men) may be the result of hormonal resistance
to testosterone. Hormonal resistance appears to happen with several hormones in
HIV pathology. However, studies suggest that the need for higher testosterone
doses is most likely caused by elevated sex-hormone binding globulins and
lowered free testosterone,
which is common in HIV.88 [xxi]
When this is the case, total testosterone measurements do not adequately
reflect the person’s state of health.
Supplementing
testosterone to bring free testosterone levels in the body into an optimal range may
be beneficial to hypogonadal men in general, by improving the partitioning
of nutrients more towards lean tissue and less toward fat tissue, especially
visceral fat.[xxii] Significant data also suggests
that appropriate testosterone supplementation can improve blood lipid chemistry
to reduce the potential for cardiovascular disease in men who are deficient.[xxiii]
testosterone to bring free testosterone levels in the body into an optimal range may
be beneficial to hypogonadal men in general, by improving the partitioning
of nutrients more towards lean tissue and less toward fat tissue, especially
visceral fat.[xxii] Significant data also suggests
that appropriate testosterone supplementation can improve blood lipid chemistry
to reduce the potential for cardiovascular disease in men who are deficient.[xxiii]
Testosterone Patches or Creams
We
have reports that application of the Testoderm TTS or Androderm testosterone patches directly on the buffalo hump appears to shrink it. If this works,
testosterone creams or gels might work better as the dose of
testosterone can be much greater than in a patch. While a study of adipocyte
(fat cell) chemistry does provide a rationale as to why application through the
skin might work, application of a cream would not be likely to work to reduce
the belly because of the greater distance from the skin through the stomach
muscles to the fat cells inside.
have reports that application of the Testoderm TTS or Androderm testosterone patches directly on the buffalo hump appears to shrink it. If this works,
testosterone creams or gels might work better as the dose of
testosterone can be much greater than in a patch. While a study of adipocyte
(fat cell) chemistry does provide a rationale as to why application through the
skin might work, application of a cream would not be likely to work to reduce
the belly because of the greater distance from the skin through the stomach
muscles to the fat cells inside.
Anabolic Steroid Improves Insulin Sensitivity and Glucose Disposal
One
study showed that the injectable anabolic steroid nandrolone decanoate (Deca
Durabolin) improved glucose disposal
and lowered insulin levels when administered at 300 mg per week,
while it did not have any effect at 100 mg.[xxiv]
While this injectable beta esterified anabolic steroid may have a beneficial
effect on insulin sensitivity another study found that it appears to enhance
non-insulin-mediated glucose disposal.[xxv]
This study and other studies state that oral 17-alpha alkylated anabolic
steroids, such as oxymetholone (Anadrol-50), oxandrolone (Oxandrin) and stanozolol (Winstrol)
promote insulin resistance because of their effect on liver metabolism.[xxvi]
[xxvii]
This raises questions about using oral steroids when lipodystrophy is present.
study showed that the injectable anabolic steroid nandrolone decanoate (Deca
Durabolin) improved glucose disposal
and lowered insulin levels when administered at 300 mg per week,
while it did not have any effect at 100 mg.[xxiv]
While this injectable beta esterified anabolic steroid may have a beneficial
effect on insulin sensitivity another study found that it appears to enhance
non-insulin-mediated glucose disposal.[xxv]
This study and other studies state that oral 17-alpha alkylated anabolic
steroids, such as oxymetholone (Anadrol-50), oxandrolone (Oxandrin) and stanozolol (Winstrol)
promote insulin resistance because of their effect on liver metabolism.[xxvi]
[xxvii]
This raises questions about using oral steroids when lipodystrophy is present.
The Paradoxical Effects of Oral Steroids
However,
oral steroids can decrease triglycerides (fats) because of
their effect of increasing post-heparin hepatic triglyceride lipase, which
breaks down triglycerides. [xxviii]
[xxix]
For this reason oral steroids may help to decrease visceral fat, although they
promote insulin resistance, and I have heard reports of each
of the oral steroids stanozolol, oxymetholone and oxandrolone reducing the
protease belly in HIV(+) males. Indeed, data from a
retrospective study of 700 patients recently released by Dr. Douglas Dieterich gave indication that the use of oral and
injectable anabolic steroids may be effective in decreasing the potential for
lipodystrophy-associated body habitus changes.[xxx]More study needs to be done to confirm
this trend, though.
oral steroids can decrease triglycerides (fats) because of
their effect of increasing post-heparin hepatic triglyceride lipase, which
breaks down triglycerides. [xxviii]
[xxix]
For this reason oral steroids may help to decrease visceral fat, although they
promote insulin resistance, and I have heard reports of each
of the oral steroids stanozolol, oxymetholone and oxandrolone reducing the
protease belly in HIV(+) males. Indeed, data from a
retrospective study of 700 patients recently released by Dr. Douglas Dieterich gave indication that the use of oral and
injectable anabolic steroids may be effective in decreasing the potential for
lipodystrophy-associated body habitus changes.[xxx]More study needs to be done to confirm
this trend, though.
Human Growth Hormone (Serostim)
While
the relative ineffectiveness of GH as a muscle-building anabolic hormone is
detailed in later sections, GH does appear to have a role in reducing
lipodystrophy because of its effect on lipid oxidation (fat burning), as was
asserted by a poster presentation from Dr. Gabriel Torres of New York, that was presented at the XII
International Conference on AIDS in Geneva.[xxxi]
the relative ineffectiveness of GH as a muscle-building anabolic hormone is
detailed in later sections, GH does appear to have a role in reducing
lipodystrophy because of its effect on lipid oxidation (fat burning), as was
asserted by a poster presentation from Dr. Gabriel Torres of New York, that was presented at the XII
International Conference on AIDS in Geneva.[xxxi]
It
should be noted that Dr. Torres said that while five patients had partial of
total reduction of fat redistribution on 5 and 6 mg doses of GH, which I assert are overdoses
for most people, four of the patients (80 percent) had either elevated glucose,
elevated pancreatic enzymes, or carpal tunnel syndrome, so GH at these doses
increased the potential for serious health problems. Elevated blood glucose can lead to diabetes and the problems that result including
cardiovascular problems, eye damage, and neuropathy; elevated pancreatic enzymes
can lead to pancreatitis; and carpal tunnel syndrome
is quite painful and may require surgery.
should be noted that Dr. Torres said that while five patients had partial of
total reduction of fat redistribution on 5 and 6 mg doses of GH, which I assert are overdoses
for most people, four of the patients (80 percent) had either elevated glucose,
elevated pancreatic enzymes, or carpal tunnel syndrome, so GH at these doses
increased the potential for serious health problems. Elevated blood glucose can lead to diabetes and the problems that result including
cardiovascular problems, eye damage, and neuropathy; elevated pancreatic enzymes
can lead to pancreatitis; and carpal tunnel syndrome
is quite painful and may require surgery.
I
suggest that if Serostim GH is implemented, it should be considered that
Serono’s full vial dose is an
overdose and this may be why 5 and 6 mg doses caused these problems. It is
advisable to adjust the dose down for each individual, in an attempt to gain
the benefit without increasing the problems. At this time I have reports of a
reduction of protease belly and other types of lipodystrophy with doses as
low as 1 mg per day and up to 3 mg per day with no side effects. I assert that
lower daily doses are safer than higher doses administered every few days, and
at a correct dose growth hormone can be an important part of the tools that
address the underlying metabolic problem. While growth hormone will have a less
powerful effect at a lower dose, at the proper individual dose there will still
be a significant effect on fat cell metabolism with significantly less
potential for side effects.
suggest that if Serostim GH is implemented, it should be considered that
Serono’s full vial dose is an
overdose and this may be why 5 and 6 mg doses caused these problems. It is
advisable to adjust the dose down for each individual, in an attempt to gain
the benefit without increasing the problems. At this time I have reports of a
reduction of protease belly and other types of lipodystrophy with doses as
low as 1 mg per day and up to 3 mg per day with no side effects. I assert that
lower daily doses are safer than higher doses administered every few days, and
at a correct dose growth hormone can be an important part of the tools that
address the underlying metabolic problem. While growth hormone will have a less
powerful effect at a lower dose, at the proper individual dose there will still
be a significant effect on fat cell metabolism with significantly less
potential for side effects.
Exercise
Exercise,
too, improves insulin sensitivity,[xxxii]
so people with insulin resistance should consider some kind of regular exercise, especially weight-training,
which also builds lean body mass. Aerobic exercise does not build significant
lean body mass. Aerobics may be useful in an effort to reduce lipodystrophy but
if a person is losing lean body mass it should be avoided at least until the
person has regained any lost weight or stabilized. Aerobics will use energy
that the body would normally use for rebuilding lean body mass, only
accelerating the loss of lean body mass. If your weight is stable and not in
danger of losing weight, to optimally burn fat and reduce lipodystrophy I
suggest doing aerobics three times per week on alternate days to
weight training days, first thing in the morning on an empty stomach. (See the
exercise chapter on page 129.)
too, improves insulin sensitivity,[xxxii]
so people with insulin resistance should consider some kind of regular exercise, especially weight-training,
which also builds lean body mass. Aerobic exercise does not build significant
lean body mass. Aerobics may be useful in an effort to reduce lipodystrophy but
if a person is losing lean body mass it should be avoided at least until the
person has regained any lost weight or stabilized. Aerobics will use energy
that the body would normally use for rebuilding lean body mass, only
accelerating the loss of lean body mass. If your weight is stable and not in
danger of losing weight, to optimally burn fat and reduce lipodystrophy I
suggest doing aerobics three times per week on alternate days to
weight training days, first thing in the morning on an empty stomach. (See the
exercise chapter on page 129.)
Nutritional Considerations
Carbohydrates
I
would also suggest altering your diet so that it is balanced somewhat like what
might be called an “evolutionary-type hunter-gatherer diet.” This means getting
more protein and a moderate amount of the healthy types of fats, while eating
fewer high-calorie, starchy, complex carbohydrates or high-glycemic, sugary,
simple carbohydrates.
would also suggest altering your diet so that it is balanced somewhat like what
might be called an “evolutionary-type hunter-gatherer diet.” This means getting
more protein and a moderate amount of the healthy types of fats, while eating
fewer high-calorie, starchy, complex carbohydrates or high-glycemic, sugary,
simple carbohydrates.
Currently,
many progressive nutritionists are recommending that people with insulin resistance consider reducing their total
calorie intake and intake of high-calorie complex carbohydrates that can
release into the blood stream quickly,[xxxiii]
including wheat breads and most processed wheat products. These kinds of
carbohydrates actually are quite calorie dense and can upset insulin metabolism
as much as sweets.[xxxiv]
[xxxv]
They are even more problematic when included in high fat foods. (Think pizza
and ice cream.) Also on the list of carbohydrates to avoid is the sugar called
fructose, which is known to promote insulin resistance, and raise cholesterol.[xxxvi]
Look for it on ingredient panels as fructose or high-fructose corn syrup. I
also underline that some people will experience a reduction in insulin
resistance just by reducing the total calories in their diet, as many people
simply eat too many calories. However, if
you are having a hard time maintaining weight because of wasting or
infection, getting plenty of healthy calories is essential for keeping and
building lean body mass, so be careful about reducing your intake of food.
many progressive nutritionists are recommending that people with insulin resistance consider reducing their total
calorie intake and intake of high-calorie complex carbohydrates that can
release into the blood stream quickly,[xxxiii]
including wheat breads and most processed wheat products. These kinds of
carbohydrates actually are quite calorie dense and can upset insulin metabolism
as much as sweets.[xxxiv]
[xxxv]
They are even more problematic when included in high fat foods. (Think pizza
and ice cream.) Also on the list of carbohydrates to avoid is the sugar called
fructose, which is known to promote insulin resistance, and raise cholesterol.[xxxvi]
Look for it on ingredient panels as fructose or high-fructose corn syrup. I
also underline that some people will experience a reduction in insulin
resistance just by reducing the total calories in their diet, as many people
simply eat too many calories. However, if
you are having a hard time maintaining weight because of wasting or
infection, getting plenty of healthy calories is essential for keeping and
building lean body mass, so be careful about reducing your intake of food.
At
the same time, I recommend an increase in the intake of complex carbohydrates
sources that contain less total calories but lots of fluid and nutrients, like
vegetables. Compared to grains, vegetables are more nutrient dense, and less
calorie dense. While some glycemic indexes vegetables like potatoes and carrots have
high, they supply good amounts of nutrients per calorie, and they do not
contain a great amount of calories for their volume like grains or sweets do,
so their effect on insulin production, insulin resistance and body fat accumulation is not as great.
(Carrots contain only 195 calories per pound, boiled potatoes contain 450
calories per pound, while breads contain about 1200 to 1500 calories per pound,
and sugar and sweets contain about 1700 calories per pound.)
the same time, I recommend an increase in the intake of complex carbohydrates
sources that contain less total calories but lots of fluid and nutrients, like
vegetables. Compared to grains, vegetables are more nutrient dense, and less
calorie dense. While some glycemic indexes vegetables like potatoes and carrots have
high, they supply good amounts of nutrients per calorie, and they do not
contain a great amount of calories for their volume like grains or sweets do,
so their effect on insulin production, insulin resistance and body fat accumulation is not as great.
(Carrots contain only 195 calories per pound, boiled potatoes contain 450
calories per pound, while breads contain about 1200 to 1500 calories per pound,
and sugar and sweets contain about 1700 calories per pound.)
Other
good carbohydrate sources are beans, yams and green peas, and whole fruits like
oranges, grapes, apples, pears, and cherries. In other words try to eat natural
food carbohydrate sources that are one step away from nature.
good carbohydrate sources are beans, yams and green peas, and whole fruits like
oranges, grapes, apples, pears, and cherries. In other words try to eat natural
food carbohydrate sources that are one step away from nature.
If
you do want to include grains in your diet, barley, cream of rye, oatmeal and
brown rice have relatively lower glycemic indexes than most wheat products, but be careful to
moderate the total amount of these high calorie starch sources. If you include
them in your diet, I suggest eating servings that are about one third as much
you’d really like to eat. (Again, try to moderate your total carbohydrate
calories if your goal is to reduce insulin resistance.)
you do want to include grains in your diet, barley, cream of rye, oatmeal and
brown rice have relatively lower glycemic indexes than most wheat products, but be careful to
moderate the total amount of these high calorie starch sources. If you include
them in your diet, I suggest eating servings that are about one third as much
you’d really like to eat. (Again, try to moderate your total carbohydrate
calories if your goal is to reduce insulin resistance.)
While
a high-carbohydrate diet has been recommended by some nutritionists for
conditions of insulin resistance (diabetes), a study by Chen of Stanford
University, showed that a lower-fat, higher-carbohydrate diet led to higher
day-long blood glucose, insulin, and triglycerides,
as well as post-prandial (after a meal) accumulation of triglycerides, and
increased VLDLs (very low density lipoproteins),[xxxvii] which can increase the risk of
cardiovascular disease. The idea that lower carbohydrates diets are superior is
supported in an article in Nutrition Reviews by dietitian Nancy Sheard, who
said, “Recent studies indicate that a
diet high in monounsaturated fat and
low in carbohydrate can produce a more desirable plasma glucose, lipid, and
insulin profile.”[xxxviii] A study published in the Journal of
the American Medical Association further supported this approach when it showed
significantly elevated triglycerides and LDL cholesterol levels with a high carbohydrate
diet, while a high-monounsaturated fat diet let to a lower-risk lipid profile.[xxxix]
a high-carbohydrate diet has been recommended by some nutritionists for
conditions of insulin resistance (diabetes), a study by Chen of Stanford
University, showed that a lower-fat, higher-carbohydrate diet led to higher
day-long blood glucose, insulin, and triglycerides,
as well as post-prandial (after a meal) accumulation of triglycerides, and
increased VLDLs (very low density lipoproteins),[xxxvii] which can increase the risk of
cardiovascular disease. The idea that lower carbohydrates diets are superior is
supported in an article in Nutrition Reviews by dietitian Nancy Sheard, who
said, “Recent studies indicate that a
diet high in monounsaturated fat and
low in carbohydrate can produce a more desirable plasma glucose, lipid, and
insulin profile.”[xxxviii] A study published in the Journal of
the American Medical Association further supported this approach when it showed
significantly elevated triglycerides and LDL cholesterol levels with a high carbohydrate
diet, while a high-monounsaturated fat diet let to a lower-risk lipid profile.[xxxix]
Fats
While
it is also best to reduce any excessive intake of fats, I don’t advocate a very
low-fat diet, but a reduction in excess saturated fats, found in animal fat
products like butter and lard, and excess omega-6 fats, which are found in common vegetable
oils, like corn, safflower, and sunflower oils. Excess saturated fats and
omega-6 fats can promote insulin resistance.115 [xl] [xli] [xlii] At the same time I recommend a
moderate intake of fresh food sources of the essential fatty acid called omega-3, which can reduce insulin
resistance,[xliii] and reduce the potential for
atherosclerosis and heart attacks.[xliv]
[xlv]
Omega-3 fats are found abundantly in cold water fish like salmon, sardines,
tuna, rainbow trout, anchovies, and herring, and in lesser amounts in flax seed
oil, some nuts and seeds and beans, like walnuts, pumpkin seeds and soy beans,
and in much smaller quantities in dark green leafy vegetables. Consider also
including some daily consumption of monounsaturated fats from sources like
olive oil. These too reduce the risk of cardiovascular disease.
it is also best to reduce any excessive intake of fats, I don’t advocate a very
low-fat diet, but a reduction in excess saturated fats, found in animal fat
products like butter and lard, and excess omega-6 fats, which are found in common vegetable
oils, like corn, safflower, and sunflower oils. Excess saturated fats and
omega-6 fats can promote insulin resistance.115 [xl] [xli] [xlii] At the same time I recommend a
moderate intake of fresh food sources of the essential fatty acid called omega-3, which can reduce insulin
resistance,[xliii] and reduce the potential for
atherosclerosis and heart attacks.[xliv]
[xlv]
Omega-3 fats are found abundantly in cold water fish like salmon, sardines,
tuna, rainbow trout, anchovies, and herring, and in lesser amounts in flax seed
oil, some nuts and seeds and beans, like walnuts, pumpkin seeds and soy beans,
and in much smaller quantities in dark green leafy vegetables. Consider also
including some daily consumption of monounsaturated fats from sources like
olive oil. These too reduce the risk of cardiovascular disease.
Data
also suggests that high saturated fat in the diet promotes more bodyfat
accumulation compared to polyunsaturated fats like omega-3 fats,[xlvi]
[xlvii]
so if you want to be lean, eat clean.
also suggests that high saturated fat in the diet promotes more bodyfat
accumulation compared to polyunsaturated fats like omega-3 fats,[xlvi]
[xlvii]
so if you want to be lean, eat clean.
Finally,
avoid eating any food that contain artificial fats or processed fats, like
hydrogenated or partially hydrogenated oils. Partially hydrogenated oils are
found in foods like margarine, french fries, potato chips, shortening, many
baked goods, and mayonnaise. Harvard researchers have found a very strong link
between these types of unhealthy fats and cardiovascular disease.[xlviii]
avoid eating any food that contain artificial fats or processed fats, like
hydrogenated or partially hydrogenated oils. Partially hydrogenated oils are
found in foods like margarine, french fries, potato chips, shortening, many
baked goods, and mayonnaise. Harvard researchers have found a very strong link
between these types of unhealthy fats and cardiovascular disease.[xlviii]
Protein
HIV
has protein malnutrition as a common theme; a lack of optimal protein
contributes to the loss of lean body mass and trouble maintaining it. To reduce
the loss of lean body mass and to increase it, I suggest that your diet include
extra protein that totals at least 3/4 gram per pound of body weight per day.
If you lift weights, studies of HIV(-) subjects by world-renowned protein
scientist Dr. Peter Lemon show that
you may need a total of at least 0.8 grams of protein per pound of body weight
per day for optimal increases in lean body mass.[xlix]
[l] If
you are not allergic to dairy protein, consider eating cottage cheese as a
“best” protein for building muscle, as it contains a great amount of the amino
acid L-glutamine, which is discussed below.
(Note: dairy allergy can cause diarrhea.)
has protein malnutrition as a common theme; a lack of optimal protein
contributes to the loss of lean body mass and trouble maintaining it. To reduce
the loss of lean body mass and to increase it, I suggest that your diet include
extra protein that totals at least 3/4 gram per pound of body weight per day.
If you lift weights, studies of HIV(-) subjects by world-renowned protein
scientist Dr. Peter Lemon show that
you may need a total of at least 0.8 grams of protein per pound of body weight
per day for optimal increases in lean body mass.[xlix]
[l] If
you are not allergic to dairy protein, consider eating cottage cheese as a
“best” protein for building muscle, as it contains a great amount of the amino
acid L-glutamine, which is discussed below.
(Note: dairy allergy can cause diarrhea.)
Also
consider supplementing your food protein with a protein powder drink two or
three times per day. Note that the dairy protein called casein, seen on labels
as calcium caseinate, appears to have the potential to be
somewhat more effective for improving lean body mass than other proteins, like
whey.[li]
consider supplementing your food protein with a protein powder drink two or
three times per day. Note that the dairy protein called casein, seen on labels
as calcium caseinate, appears to have the potential to be
somewhat more effective for improving lean body mass than other proteins, like
whey.[li]
The Zone Diet
Although
I do not agree with some of his more dogmatic concepts, my recommendations for
nutrition have some similarities to the “zone” diet outlined in the book Mastering the Zone, by Dr. Barry Sears. While aspects of the zone
diet can be criticized scientifically, I have had numerous reports that the use
of the zone diet has helped people with HIV reduce cholesterol, the potbelly,
triglycerides, and lipodystrophy symptoms, in general.
I do not agree with some of his more dogmatic concepts, my recommendations for
nutrition have some similarities to the “zone” diet outlined in the book Mastering the Zone, by Dr. Barry Sears. While aspects of the zone
diet can be criticized scientifically, I have had numerous reports that the use
of the zone diet has helped people with HIV reduce cholesterol, the potbelly,
triglycerides, and lipodystrophy symptoms, in general.
The Atkins Diet
The
Atkins diet is a very low carbohydrate, high protein, high fat diet that can
decrease bodyfat significantly. I have reports of people successfully using the
Atkins diet to reduce lipodystrophy symptoms. Consider that it is basically
impossible to get the RDA of vitamins, minerals or fiber from this diet, so if
you use it, take strong multi-vitamins and extra fiber, and consider that it
shouldn’t be used long-term. Also be sure to favor monounsaturated and omega-3 fats over omega-6 and saturated fats.
Atkins diet is a very low carbohydrate, high protein, high fat diet that can
decrease bodyfat significantly. I have reports of people successfully using the
Atkins diet to reduce lipodystrophy symptoms. Consider that it is basically
impossible to get the RDA of vitamins, minerals or fiber from this diet, so if
you use it, take strong multi-vitamins and extra fiber, and consider that it
shouldn’t be used long-term. Also be sure to favor monounsaturated and omega-3 fats over omega-6 and saturated fats.
Dietary Supplements
Supplements
that have been shown to improve insulin sensitivity include chromium,[lii]
and I recommend 200 to 400 micrograms (mcg) of chromium three times per day in
the polynicotinate or picolinate form, as one recent (non-HIV) study showed
that 1,000 mcg of chromium per day increased insulin sensitivity by about 40
percent without toxicity.[liii]
that have been shown to improve insulin sensitivity include chromium,[lii]
and I recommend 200 to 400 micrograms (mcg) of chromium three times per day in
the polynicotinate or picolinate form, as one recent (non-HIV) study showed
that 1,000 mcg of chromium per day increased insulin sensitivity by about 40
percent without toxicity.[liii]
The
herb silymarin (milk thistle) as a standardized extract in
a dose of 200 mg three times per day has been shown to be effective in
improving liver function and improving insulin sensitivity.[liv]
There has been talk that silymarin can alter liver function in a way that might
affect the metabolism of protease inhibitors, so it is possible that people who
are taking protease inhibitors should not take silymarin. There is no
conclusive data on this yet.
herb silymarin (milk thistle) as a standardized extract in
a dose of 200 mg three times per day has been shown to be effective in
improving liver function and improving insulin sensitivity.[liv]
There has been talk that silymarin can alter liver function in a way that might
affect the metabolism of protease inhibitors, so it is possible that people who
are taking protease inhibitors should not take silymarin. There is no
conclusive data on this yet.
But
the best supplement for improving insulin sensitivity and glucose disposal may be the antioxidant
called alpha lipoic acid (ALA), at 100 to 300 mg three
times per day.[lv]
In diabetic studies ALA improves insulin dependent and non-insulin dependent
glucose uptake, and it has been shown to effectively lower blood sugar
comparable to insulin itself.[lvi]
I believe this is one very important reason ALA is a must for anyone taking HIV
medications, especially protease inhibitors. HIV-nutrition expert Lark Lands, Ph.D., asserts that ALA is a
must for people with HIV because of its effect on improving glutathione production and recycling.[lvii]
Studies last year at Stanford University showed that glutathione levels
directly correlate with increased survival for people with HIV.[lviii]
the best supplement for improving insulin sensitivity and glucose disposal may be the antioxidant
called alpha lipoic acid (ALA), at 100 to 300 mg three
times per day.[lv]
In diabetic studies ALA improves insulin dependent and non-insulin dependent
glucose uptake, and it has been shown to effectively lower blood sugar
comparable to insulin itself.[lvi]
I believe this is one very important reason ALA is a must for anyone taking HIV
medications, especially protease inhibitors. HIV-nutrition expert Lark Lands, Ph.D., asserts that ALA is a
must for people with HIV because of its effect on improving glutathione production and recycling.[lvii]
Studies last year at Stanford University showed that glutathione levels
directly correlate with increased survival for people with HIV.[lviii]
As
noted by the late Canadian protein chemist Chester Myers, Ph.D., N-acetyl cysteine
(NAC) can be a valuable addition to the supplements
that address lipodystrophy, because of its effect on improving glutathione, which is necessary for
glucose metabolism. I suggest 500 to 1,000 mg of NAC three times per day.
noted by the late Canadian protein chemist Chester Myers, Ph.D., N-acetyl cysteine
(NAC) can be a valuable addition to the supplements
that address lipodystrophy, because of its effect on improving glutathione, which is necessary for
glucose metabolism. I suggest 500 to 1,000 mg of NAC three times per day.
Also
carnitine, as the prescription version
called Carnitor, would be beneficial in
higher doses, about 500 to 1,000 mg three times per day, as it helps to lower
triglycerides,[lix]
which are generally elevated when lipodystrophy is present. Note that the
acetyl-L-carnitine form of carnitine may be more effective than
plain carnitine, but it is more expensive.
carnitine, as the prescription version
called Carnitor, would be beneficial in
higher doses, about 500 to 1,000 mg three times per day, as it helps to lower
triglycerides,[lix]
which are generally elevated when lipodystrophy is present. Note that the
acetyl-L-carnitine form of carnitine may be more effective than
plain carnitine, but it is more expensive.
Also worth
considering is the omega-3 dietary supplement called EPA (fish oil), which has been shown to reduce
insulin resistance,115 and lower triglycerides somewhat in a study
with HIV(+) men.[lx]
considering is the omega-3 dietary supplement called EPA (fish oil), which has been shown to reduce
insulin resistance,115 and lower triglycerides somewhat in a study
with HIV(+) men.[lx]
And
taking a strong multivitamin, multimineral supplement that includes chromium, vitamins A, D, E and calcium and magnesium will help improve insulin sensitivity.[lxi] [lxii]
[lxiii]
[lxiv]
[lxv] [lxvi]
I recommend taking a supplement that contains doses that are much higher than
the RDAs, though, as numerous studies have shown that higher nutrient levels
are required in HIV disease.[lxvii] [lxviii]
taking a strong multivitamin, multimineral supplement that includes chromium, vitamins A, D, E and calcium and magnesium will help improve insulin sensitivity.[lxi] [lxii]
[lxiii]
[lxiv]
[lxv] [lxvi]
I recommend taking a supplement that contains doses that are much higher than
the RDAs, though, as numerous studies have shown that higher nutrient levels
are required in HIV disease.[lxvii] [lxviii]
Finally,
high dose biotin supplementation is frequently prescribed by
nutritionally-oriented medical doctors to improve glucose metabolism in
diabetes.[lxix]
[lxx]
High dose biotin is also known to improve diabetic neuropathy.[lxxi]
The dose of biotin that is commonly used is 1,000 mcg three times per day.
high dose biotin supplementation is frequently prescribed by
nutritionally-oriented medical doctors to improve glucose metabolism in
diabetes.[lxix]
[lxx]
High dose biotin is also known to improve diabetic neuropathy.[lxxi]
The dose of biotin that is commonly used is 1,000 mcg three times per day.
Cardiovascular Disease
As I
mentioned in the beginning of this article, we are also beginning to see
cardiovascular disease in people on protease inhibitors. When cardiovascular
disease is a consideration, we want to make sure that specific preventive
nutrients are included. While there are many that can be included for this
purpose, to keep it simple I suggest the following: vitamin E at 400 to 800 IU
three times per day to reduce the potential for oxidation of blood fats that
can contribute to atherosclerosis;[lxxii]
vitamin C at 1,000 to 2,000 mg three times per day to assist vitamin E in
reducing blood fat oxidation;[lxxiii]
folic acid at 800 mcg three times per day to reduce the
potential for elevated homocysteine, which appears to be another
major contributory factor to cardiovascular disease.[lxxiv]
[lxxv]
It should also be noted that vitamins B6 at 50 mg three times per day and
vitamin B12 at 100 to 500 mcg three times per day help to reduce homocysteine.
Of course, all HIV(+) people should consider taking high doses of supplemental
B vitamins, as studies by Dr. Marianna Baum, of the University of Miami, showed
that HIV(+) people frequently require 6 to 25 times the RDA of these essential
nutrients to stay healthy.139 140
mentioned in the beginning of this article, we are also beginning to see
cardiovascular disease in people on protease inhibitors. When cardiovascular
disease is a consideration, we want to make sure that specific preventive
nutrients are included. While there are many that can be included for this
purpose, to keep it simple I suggest the following: vitamin E at 400 to 800 IU
three times per day to reduce the potential for oxidation of blood fats that
can contribute to atherosclerosis;[lxxii]
vitamin C at 1,000 to 2,000 mg three times per day to assist vitamin E in
reducing blood fat oxidation;[lxxiii]
folic acid at 800 mcg three times per day to reduce the
potential for elevated homocysteine, which appears to be another
major contributory factor to cardiovascular disease.[lxxiv]
[lxxv]
It should also be noted that vitamins B6 at 50 mg three times per day and
vitamin B12 at 100 to 500 mcg three times per day help to reduce homocysteine.
Of course, all HIV(+) people should consider taking high doses of supplemental
B vitamins, as studies by Dr. Marianna Baum, of the University of Miami, showed
that HIV(+) people frequently require 6 to 25 times the RDA of these essential
nutrients to stay healthy.139 140
Glutamine
For
any loss of muscle, Judy Shabert,
M.D., M.P.H., R.D., asserts that supplementing with high doses of the amino
acid L-glutamine, will help reduce the
catabolic process of breaking down muscle tissue,[lxxvi]
and a recent study of wasting HIV patients by Prang showed that this might be true. (See Dr.
Shabert’s article in the August 1997 issue of POZ magazine.) For frank wasting,
HIV(+) people are using between 12 and 36 grams per day of L-glutamine. (One
tablespoon is 12 grams.) I have friends who have halted their random diarrhea and improved their lean body mass using these
kinds of L-glutamine doses, and in Prang’s study wasting and diarrhea and were
checked by using 30 to 40 grams of glutamine per day. Glutamine too, has been
shown to have a powerful effect on improving glutathione production,[lxxvii]
and glutamine improves insulin sensitivity.[lxxviii]
[lxxix]
any loss of muscle, Judy Shabert,
M.D., M.P.H., R.D., asserts that supplementing with high doses of the amino
acid L-glutamine, will help reduce the
catabolic process of breaking down muscle tissue,[lxxvi]
and a recent study of wasting HIV patients by Prang showed that this might be true. (See Dr.
Shabert’s article in the August 1997 issue of POZ magazine.) For frank wasting,
HIV(+) people are using between 12 and 36 grams per day of L-glutamine. (One
tablespoon is 12 grams.) I have friends who have halted their random diarrhea and improved their lean body mass using these
kinds of L-glutamine doses, and in Prang’s study wasting and diarrhea and were
checked by using 30 to 40 grams of glutamine per day. Glutamine too, has been
shown to have a powerful effect on improving glutathione production,[lxxvii]
and glutamine improves insulin sensitivity.[lxxviii]
[lxxix]
If
you are losing weight I suggest that you supplement your diet with a tablespoon
of L-glutamine added to each serving of supplemental protein
two or three times per day between meals. If your weight is stable, L-glutamine
may be supplemented at lower doses, such as one or more teaspoons per day.
you are losing weight I suggest that you supplement your diet with a tablespoon
of L-glutamine added to each serving of supplemental protein
two or three times per day between meals. If your weight is stable, L-glutamine
may be supplemented at lower doses, such as one or more teaspoons per day.
(Important
note: most dietary supplements only stay in the blood for a few hours, so it is
wise to take them several times per day.)
note: most dietary supplements only stay in the blood for a few hours, so it is
wise to take them several times per day.)
Metformin (Glucophage)
Realize
that while taking dietary supplements, especially alpha lipoic acid, may help,
it is wise to investigate the use of the drugs that are prescribed to improve insulin sensitivity. Ask your doctor about these
drugs, which include metformin.[lxxx] New data presented by Saint-Marc at
the 6th Retrovirus Conference, in February, 1999 indicates that metformin may
decrease visceral fat while decreasing blood glucose, insulin, and lipid levels. 102 Serostim can increase blood glucose, insulin and
insulin resistance.[lxxxi] [lxxxii] This means that metformin might be
found to be superior to Serostim growth hormone because it not only addresses
fat redistribution, but reduces some of the underlying metabolic problems that
growth hormone can promote. An important consideration is that while 6 mg per
day of Serostim is priced at about $6,000 per month, which makes it
inaccessible for a majority of people who have lipodystrophy, metformin is
available with a doctor’s prescription at any pharmacy, and if a person has to
pay for it themselves. Realize that while taking dietary supplements,
especially alpha lipoic acid, may help, it is wise to investigate the use of
the drugs that are prescribed to improve insulin sensitivity. Ask your doctor
about these drugs, which include metformin.152 New data presented by Saint-Marc at the 6th
Retrovirus Conference, in February, 1999 indicates that metformin may decrease
visceral fat while decreasing blood glucose, insulin, and lipid levels.102 Serostim can increase blood glucose, insulin
and insulin resistance.153 154 This
means that metformin might be found to be superior to Serostim growth hormone
because it not only addresses fat redistribution, but reduces some of the
underlying metabolic problems that growth hormone can promote. An important
consideration is that while Serostim is priced at $6,000 per month, which makes
it inaccessible for a majority of people who have lipodystrophy, metformin is
available with a doctor’s prescription at any pharmacy, and if a person has to
pay for it themselves, it only costs about $35 per month.
that while taking dietary supplements, especially alpha lipoic acid, may help,
it is wise to investigate the use of the drugs that are prescribed to improve insulin sensitivity. Ask your doctor about these
drugs, which include metformin.[lxxx] New data presented by Saint-Marc at
the 6th Retrovirus Conference, in February, 1999 indicates that metformin may
decrease visceral fat while decreasing blood glucose, insulin, and lipid levels. 102 Serostim can increase blood glucose, insulin and
insulin resistance.[lxxxi] [lxxxii] This means that metformin might be
found to be superior to Serostim growth hormone because it not only addresses
fat redistribution, but reduces some of the underlying metabolic problems that
growth hormone can promote. An important consideration is that while 6 mg per
day of Serostim is priced at about $6,000 per month, which makes it
inaccessible for a majority of people who have lipodystrophy, metformin is
available with a doctor’s prescription at any pharmacy, and if a person has to
pay for it themselves. Realize that while taking dietary supplements,
especially alpha lipoic acid, may help, it is wise to investigate the use of
the drugs that are prescribed to improve insulin sensitivity. Ask your doctor
about these drugs, which include metformin.152 New data presented by Saint-Marc at the 6th
Retrovirus Conference, in February, 1999 indicates that metformin may decrease
visceral fat while decreasing blood glucose, insulin, and lipid levels.102 Serostim can increase blood glucose, insulin
and insulin resistance.153 154 This
means that metformin might be found to be superior to Serostim growth hormone
because it not only addresses fat redistribution, but reduces some of the
underlying metabolic problems that growth hormone can promote. An important
consideration is that while Serostim is priced at $6,000 per month, which makes
it inaccessible for a majority of people who have lipodystrophy, metformin is
available with a doctor’s prescription at any pharmacy, and if a person has to
pay for it themselves, it only costs about $35 per month.
However,
cautions about the use of metformin are warranted. Dr. Michael Dube, of the University of
Southern California at Los Angeles says, “Lactic
acidosis is a
rare side effect of metformin that is more likely to occur when there is some
impairment of kidney function. Lactic acidosis, which can be fatal, is also a
rare side effect of use of nucleoside analogs. There is no way to know at this
time if using the two together might result in more frequent, or more severe
lactic acidosis problems. In my opinion anyway, metformin and NRTI’s therefore
should only be used together with great caution. Also, keep in mind that
metformin can lower vitamin B12 levels.”
cautions about the use of metformin are warranted. Dr. Michael Dube, of the University of
Southern California at Los Angeles says, “Lactic
acidosis is a
rare side effect of metformin that is more likely to occur when there is some
impairment of kidney function. Lactic acidosis, which can be fatal, is also a
rare side effect of use of nucleoside analogs. There is no way to know at this
time if using the two together might result in more frequent, or more severe
lactic acidosis problems. In my opinion anyway, metformin and NRTI’s therefore
should only be used together with great caution. Also, keep in mind that
metformin can lower vitamin B12 levels.”
I
should also note that some people are finding that switching antivirals causes
a marked reduction in some lipodystrophy symptoms. This is an area that is
currently receiving a considerable amount of study.
should also note that some people are finding that switching antivirals causes
a marked reduction in some lipodystrophy symptoms. This is an area that is
currently receiving a considerable amount of study.
For a good
and simple brochure on lipodystrophy, visit https://www.vhconcepts.com/pdfs/2002.changes.pdf
. For an update of lipodystrophy issues go to www.medibolics.com , www.powerusa.org and subscribe to
Nelson’s free email list by sending a blank email to p[email protected]
and simple brochure on lipodystrophy, visit https://www.vhconcepts.com/pdfs/2002.changes.pdf
. For an update of lipodystrophy issues go to www.medibolics.com , www.powerusa.org and subscribe to
Nelson’s free email list by sending a blank email to p[email protected]
[i] Karnieli, E, et al. Insulin
resistance in Cushing’s syndrome. Horm Metab Res (1985)
17(10):518-521.
resistance in Cushing’s syndrome. Horm Metab Res (1985)
17(10):518-521.
[ii] Oehler, G, et al. Hyperinsulinaemia
and impaired glucose tolerance in chronic inflammatory liver disease (author’s
disease). Z Gastroenterol (1981) 19(1):26-32.
and impaired glucose tolerance in chronic inflammatory liver disease (author’s
disease). Z Gastroenterol (1981) 19(1):26-32.
[iii]
Laakso, M, Insulin
resistance and coronary heart disease. Curr Opin Lipidol (1996) 7(4):217-226.
Laakso, M, Insulin
resistance and coronary heart disease. Curr Opin Lipidol (1996) 7(4):217-226.
[iv]
Bjórntorp, P. The
regulation of adipose tissue distribution in humans. Int J Obes Relat Metab
Disord (1996) 20(4):291-302.
Bjórntorp, P. The
regulation of adipose tissue distribution in humans. Int J Obes Relat Metab
Disord (1996) 20(4):291-302.
[v] Mulligan, KE, et al. Evidence of unique metabolic
effects of protease inhibitors. 5th Conf Retrovir Oppor Infect (1998) Feb
_1-5;157 (Abstract No. 414).
effects of protease inhibitors. 5th Conf Retrovir Oppor Infect (1998) Feb
_1-5;157 (Abstract No. 414).
[vi] Walli, RK, et al. Peripheral insulin resistance leading to impaired glucose
tolerance in HIV-1 infected patients treated with protease inhibitors. Int Conf
AIDS, Geneva (1998)12:777 (Abstract No. 179/41177).
tolerance in HIV-1 infected patients treated with protease inhibitors. Int Conf
AIDS, Geneva (1998)12:777 (Abstract No. 179/41177).
[vii] Carr, A, et al. Pathogenesis of HIV-1
protease inhibitor-associated peripheral
lipodystrophy, hyperlipidaemia, and insulin resistance. Lancet (1998) Jun 20;351(9119):1881-1883.
protease inhibitor-associated peripheral
lipodystrophy, hyperlipidaemia, and insulin resistance. Lancet (1998) Jun 20;351(9119):1881-1883.
[viii] Haffner, SM. Decreased
testosterone and dehydroepiandrosterone sulfate concentrations are associated with
increased insulin and glucose concentrations in nondiabetic men.
Metabol (1994) 43(5):599-603.
testosterone and dehydroepiandrosterone sulfate concentrations are associated with
increased insulin and glucose concentrations in nondiabetic men.
Metabol (1994) 43(5):599-603.
[ix]
Haffner, SM. Decreased testosterone and dehydroepiandrosterone sulfate concentrations are associated with
increased insulin and glucose concentrations in nondiabetic men.
Metabol (1994) 43(5):599-603.
Haffner, SM. Decreased testosterone and dehydroepiandrosterone sulfate concentrations are associated with
increased insulin and glucose concentrations in nondiabetic men.
Metabol (1994) 43(5):599-603.
[x] Armellini, F, et al. Interrelationships between intraabdominal fat and
total serum testosterone levels in obese
women. Metabolism
(1994) 43(3):390-5.
total serum testosterone levels in obese
women. Metabolism
(1994) 43(3):390-5.
[xi] Engelson, ES, et al. Nutrition and
testosterone status in HIV-positive women. XI International Conference on AIDS, Vancouver
(1996) Abstract Tu. B.2382.
testosterone status in HIV-positive women. XI International Conference on AIDS, Vancouver
(1996) Abstract Tu. B.2382.
[xii] Benbrik, E, et al. Cellular and
mitochondrial toxicity of zidovudine (AZT) didanosine (ddI) and zalcitabine
(ddC) on cultured human muscle cells. J Neurol Sci (1997) 149(1):19-25.
mitochondrial toxicity of zidovudine (AZT) didanosine (ddI) and zalcitabine
(ddC) on cultured human muscle cells. J Neurol Sci (1997) 149(1):19-25.
[xiii] Kotler, DP, et al. Magnitude of
body-cell-mass depletion and the timing of death from wasting in AIDS. Am J Clin Nutr (1989) 50:444-447.
body-cell-mass depletion and the timing of death from wasting in AIDS. Am J Clin Nutr (1989) 50:444-447.
[xiv] Greene, JB, et al. Clinical
approach to weight loss in the patient with HIV infections. Gastro Clinics of
No Amer (1988) 17(3):573-576.
approach to weight loss in the patient with HIV infections. Gastro Clinics of
No Amer (1988) 17(3):573-576.
[xv] Hellerstein, MK, et al. Increased de novo
hepatic lipogenesis in human immunodeficiency virus infection. J Clin Endocrinol Metab (1993) 76(3):559-565.
hepatic lipogenesis in human immunodeficiency virus infection. J Clin Endocrinol Metab (1993) 76(3):559-565.
[xvi] Laudat, A, et al. Changes in
systemic gonadal and adrenal steroids in asymptomatic human immunodeficiency
virus-infected men: relationship with the CD4 cell counts. Eur J Endocrinol (1995) 133(4):418-424.
systemic gonadal and adrenal steroids in asymptomatic human immunodeficiency
virus-infected men: relationship with the CD4 cell counts. Eur J Endocrinol (1995) 133(4):418-424.
[xvii] Grinspoon, SC, et al. Loss of lean body and
muscle mass correlates with androgen levels in hypogonadal men with acquired immunodeficiency syndrome
and wasting. J Clin Endocrinol Metab (1996) 81(11):4051-4058.
muscle mass correlates with androgen levels in hypogonadal men with acquired immunodeficiency syndrome
and wasting. J Clin Endocrinol Metab (1996) 81(11):4051-4058.
[xviii] Grinspoon, SC, et al. Body composition and
endocrine function in women with acquired immunodeficiency syndrome wasting. J Clin Endocrinol Metab
(1997) 82(5):1332-1337.
endocrine function in women with acquired immunodeficiency syndrome wasting. J Clin Endocrinol Metab
(1997) 82(5):1332-1337.
[xix]
Parsch, CJ, et al. Injectable testosterone undecanoate has more favourable
pharmacokinetics and pharmacodynamics than testosterone enanthate. Euro J of
Endo (1995) 132:514-519.
Parsch, CJ, et al. Injectable testosterone undecanoate has more favourable
pharmacokinetics and pharmacodynamics than testosterone enanthate. Euro J of
Endo (1995) 132:514-519.
[xx] Rabkin, JG, et al. Testosterone
replacement therapy for HIV-infected men. The AIDS Reader (1995)
July/August:136-144.
replacement therapy for HIV-infected men. The AIDS Reader (1995)
July/August:136-144.
[xxi] Martin, ME, et al. Alterations in
the concentrations and binding properties of sex steroid binding protein and
corticosteroid-binding globulin in HIV-positive patients. J Endocrinol Invest (1992) 15(8):597-603.
the concentrations and binding properties of sex steroid binding protein and
corticosteroid-binding globulin in HIV-positive patients. J Endocrinol Invest (1992) 15(8):597-603.
[xxii] Marin, P, et al. Androgen replacement of middle aged, obese men:
effects on metabolism, muscle, and adipose tissues. Eur J Med (1992) 1(6):329-336.
effects on metabolism, muscle, and adipose tissues. Eur J Med (1992) 1(6):329-336.
[xxiii]
Moller, J. Cholesterol: Interactions with Testosterone and Cortisol in
Cardiovascular Disease, Springer-Verlag; Berlin (1987).
Moller, J. Cholesterol: Interactions with Testosterone and Cortisol in
Cardiovascular Disease, Springer-Verlag; Berlin (1987).
[xxiv]
Friedl, KE, et al. The administration of pharmacological doses of testosterone or 19-nortestosterone to normal men is not
associated with increased insulin secretion or impaired glucose tolerance. J
Clin Endocrinol Metab (1989) May 68(5):971-5.
Friedl, KE, et al. The administration of pharmacological doses of testosterone or 19-nortestosterone to normal men is not
associated with increased insulin secretion or impaired glucose tolerance. J
Clin Endocrinol Metab (1989) May 68(5):971-5.
[xxv] Hobbs, CJ, et al. Nandrolone, a
19-nortestosterone, enhances insulin-independent glucose uptake in
normal men. [see comments] J Clin Endocrinol Metab (1996) 81(4):1582-1585.
19-nortestosterone, enhances insulin-independent glucose uptake in
normal men. [see comments] J Clin Endocrinol Metab (1996) 81(4):1582-1585.
[xxvi] Woodard, TL, et al. Glucose
intolerance and insulin resistance in aplastic anemia treated with
oxymetholone. J Clin Endocrinol Metab (1981) 53(5):905-908.
intolerance and insulin resistance in aplastic anemia treated with
oxymetholone. J Clin Endocrinol Metab (1981) 53(5):905-908.
[xxvii]
Kailin, X, et al. Hyperinsulinemia accompanying hyperglycemia in Chinese patients with aplastic anemia. Am J
Hematol (1997) 56(3):151-4.
Kailin, X, et al. Hyperinsulinemia accompanying hyperglycemia in Chinese patients with aplastic anemia. Am J
Hematol (1997) 56(3):151-4.
[xxviii] Kantor, MA, et al. Androgens
reduce HDL2-cholesterol and increase hepatic triglyceride lipase activity. Med
Sci Sports Exerc (1985) 17(4):462-5.
reduce HDL2-cholesterol and increase hepatic triglyceride lipase activity. Med
Sci Sports Exerc (1985) 17(4):462-5.
[xxix]
Applebaum-Bowden D, et al. The dyslipoproteinemia of anabolic steroid therapy:
increase in hepatic triglyceride lipase precedes the decrease in high-density
lipoprotein 2 cholesterol. Metab (1987) 36(10):949-952.
Applebaum-Bowden D, et al. The dyslipoproteinemia of anabolic steroid therapy:
increase in hepatic triglyceride lipase precedes the decrease in high-density
lipoprotein 2 cholesterol. Metab (1987) 36(10):949-952.
[xxx]
Dieterich, D, et al. Incidence of body
habitus changes in a cohort of 700 HIV-infected patients. Infect Diseases Soc
Amer (1998) Nov 12 – 15. Abstract No. 477.
Dieterich, D, et al. Incidence of body
habitus changes in a cohort of 700 HIV-infected patients. Infect Diseases Soc
Amer (1998) Nov 12 – 15. Abstract No. 477.
[xxxi] Torres, RA, et al. Treatment of
dorsocervical fat pads (buffalo hump) and truncal obesity with Serostim (recombinant human growth hormone) in patients with AIDS
maintained on HAART. XII International AIDS Conference, Geneva (1998) June
28-July 3. Abstract No. 32164.
dorsocervical fat pads (buffalo hump) and truncal obesity with Serostim (recombinant human growth hormone) in patients with AIDS
maintained on HAART. XII International AIDS Conference, Geneva (1998) June
28-July 3. Abstract No. 32164.
[xxxii] Henricksson, J, et al. Influence of exercise on insulin sensitivity. J
Cardio Risk (1995) 2(4):303-309.
Cardio Risk (1995) 2(4):303-309.
[xxxiii] McCarty, MF, et al. Reduction of
free fatty acids may ameliorate risk factors associated with abdominal obesity.
Med Hypotheses (1995) 44(4):278-286.
free fatty acids may ameliorate risk factors associated with abdominal obesity.
Med Hypotheses (1995) 44(4):278-286.
[xxxiv]
Truswell, AS. Food carbohydrates and plasma lipids — an update. Am J Clin Nutr
(1994) 59(suppl)(3):S710S-S718.
Truswell, AS. Food carbohydrates and plasma lipids — an update. Am J Clin Nutr
(1994) 59(suppl)(3):S710S-S718.
[xxxv] Miller, JC, et al. Replacing
starch with sucrose in a high glycaemic index breakfast cereal lowers glycaemic
and insulin responses. Eur J Clin Nutr (1994) 48(10):749-752.
starch with sucrose in a high glycaemic index breakfast cereal lowers glycaemic
and insulin responses. Eur J Clin Nutr (1994) 48(10):749-752.
[xxxvi] Pamies-Andreu, E, et al. High-fructose
feeding elicits insulin resistance without hypertension in normal
mongrel dogs. Am J Hypertens (1995) 8(7):732-738.
feeding elicits insulin resistance without hypertension in normal
mongrel dogs. Am J Hypertens (1995) 8(7):732-738.
[xxxvii] Chen, YD, et al. Why do low-fat
high-carbohydrate diets accentuate postprandial lipemia in patients with NIDDM?
Diabetes Care (1995) 18(1):10-16.
high-carbohydrate diets accentuate postprandial lipemia in patients with NIDDM?
Diabetes Care (1995) 18(1):10-16.
[xxxviii]
Sheard, NF. The diabetic diet: evidence for a new approach. Nutr Rev (1995) 53(1):16-18.
Sheard, NF. The diabetic diet: evidence for a new approach. Nutr Rev (1995) 53(1):16-18.
[xxxix] Garg, A, et al. Effects of varying
carbohydrate content of diet in patients with non-insulin-dependent diabetes mellitus [see comments]. JAMA (1994) 271(18):1421-1428.
carbohydrate content of diet in patients with non-insulin-dependent diabetes mellitus [see comments]. JAMA (1994) 271(18):1421-1428.
[xl] Storlien, LH, et al. Influence of dietary fat composition on development
of insulin resistance in rats. Relationship to muscle
triglyceride and omega-3 fatty acids in muscle phospholipid. Diabetes
(1991) 40(2):280-289.
of insulin resistance in rats. Relationship to muscle
triglyceride and omega-3 fatty acids in muscle phospholipid. Diabetes
(1991) 40(2):280-289.
[xli]
Berry, EM. Dietary fatty
acids in the management of diabetes mellitus. Am J Clin Nutr (1997) 66(4
Suppl):991S-997S.
Berry, EM. Dietary fatty
acids in the management of diabetes mellitus. Am J Clin Nutr (1997) 66(4
Suppl):991S-997S.
[xlii] Yam, D, et al. Diet
and disease—the Israeli paradox: possible dangers of a high omega-6 polyunsaturated fatty acid diet. Isr J Med Sci
(1996) 32(11):1134-1143.
and disease—the Israeli paradox: possible dangers of a high omega-6 polyunsaturated fatty acid diet. Isr J Med Sci
(1996) 32(11):1134-1143.
[xliii] Liu, S, et al. Dietary omega-3 and polyunsaturated fatty acids modify fatty
acid composition and insulin binding in skeletal-muscle sarcolemma. Biochem
J (1994) 299 (pt 3):831-837.
acid composition and insulin binding in skeletal-muscle sarcolemma. Biochem
J (1994) 299 (pt 3):831-837.
[xliv] Ponte, E, et al. Cardiovascular disease and omega-3 fatty acids. Minerva Med
(1997) 88(9):343-53.
(1997) 88(9):343-53.
[xlv] Mori, TA, et al. Interactions
between dietary fat, fish, and fish oils and their effects on platelet function
in men at risk of cardiovascular disease. Arterioscler Thromb Vasc Biol (1997)
17(2):279-286.
between dietary fat, fish, and fish oils and their effects on platelet function
in men at risk of cardiovascular disease. Arterioscler Thromb Vasc Biol (1997)
17(2):279-286.
[xlvi] Tatsuhiro, M, et al., et al. Beef
tallow diet decreases lipoprotein lipase activities in brown adipose tissue,
heart, and soleus muscle in reducing sympathetic activities in rats. J Nutr Sci Vitaminol (1994) _40:569-581
tallow diet decreases lipoprotein lipase activities in brown adipose tissue,
heart, and soleus muscle in reducing sympathetic activities in rats. J Nutr Sci Vitaminol (1994) _40:569-581
[xlvii]
Okuno M, et al., Perilla oil prevents the excessive growth of visceral adipose
tissue in rats by down-regulating adipocyte differentiation. J Nutr (1997)
127(9):1752-1757.
Okuno M, et al., Perilla oil prevents the excessive growth of visceral adipose
tissue in rats by down-regulating adipocyte differentiation. J Nutr (1997)
127(9):1752-1757.
[xlviii]
Ascherio, A, et al. Health effects of trans fatty acids. Am J Clin Nutr (1997)
66(4 Suppl):1006S-1010S.
Ascherio, A, et al. Health effects of trans fatty acids. Am J Clin Nutr (1997)
66(4 Suppl):1006S-1010S.
[xlix] Lemon, PW, et al.
Do athletes need
more dietary protein and amino acids? Int J Sports Nutri (1995) 5:S39-S61.
Do athletes need
more dietary protein and amino acids? Int J Sports Nutri (1995) 5:S39-S61.
[l] Lemon, PW, et al.
Protein requirements
and muscle mass strength changes during intensive training in novice
bodybuilders. J Appl Physiol (1992) 73(2):767-775.
Protein requirements
and muscle mass strength changes during intensive training in novice
bodybuilders. J Appl Physiol (1992) 73(2):767-775.
[li] Boirie, Y, et al. Slow
and fast dietary proteins differently modulate postprandial protein accretion.
Proceedings of the National Academy of Science USA (1997) 94: 14930-14935.
and fast dietary proteins differently modulate postprandial protein accretion.
Proceedings of the National Academy of Science USA (1997) 94: 14930-14935.
[lii]
Wilson, BE, et al. Effects of chromium supplementation on fasting insulin levels and lipid parameters in healthy,
non-obese young subjects. Diabetes
Res Clin Pract (1995) 28(3):179-184.
Wilson, BE, et al. Effects of chromium supplementation on fasting insulin levels and lipid parameters in healthy,
non-obese young subjects. Diabetes
Res Clin Pract (1995) 28(3):179-184.
[liii] Anderson, RA, et al. Elevated
intake of supplemental chromium improves glucose and insulin variables in individuals with type 2 diabetes. Diabetes (1997) 46:1786-1791.
intake of supplemental chromium improves glucose and insulin variables in individuals with type 2 diabetes. Diabetes (1997) 46:1786-1791.
[liv] Velussi, M, et al. Long-term (12
months) treatment with an antioxidant drug (silymarin) is effective on
hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic
diabetic patients. J of Hepatol (1997) 26:871-879.
months) treatment with an antioxidant drug (silymarin) is effective on
hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic
diabetic patients. J of Hepatol (1997) 26:871-879.
[lv]
Jacobs, S, et al. Enhancement of glucose disposal in patients with type 2
diabetes by
alpha-lipoic acid. Drug Res (1995)
45:872-874.
Jacobs, S, et al. Enhancement of glucose disposal in patients with type 2
diabetes by
alpha-lipoic acid. Drug Res (1995)
45:872-874.
[lvi] Estrada, EH, et al. Stimulation of
glucose uptake by the natural coenzyme a-lipoic acid/thioctic acid. Diabetes (1996) 45:1798-1804.
glucose uptake by the natural coenzyme a-lipoic acid/thioctic acid. Diabetes (1996) 45:1798-1804.
[lvii] Busse, E, et al. Influence of
alpha-lipoic acid on intracellular glutathione in vitro and in vivo. Arzneimittel-Forshung
(1992) 42:829-831.
alpha-lipoic acid on intracellular glutathione in vitro and in vivo. Arzneimittel-Forshung
(1992) 42:829-831.
[lviii]
Herzenberg L, et al. Glutathione deficiency is associated with impaired
survival in HIV disease. Proceedings of the National Academy of Sciences USA
(1997) 94(5):1967-1972.
Herzenberg L, et al. Glutathione deficiency is associated with impaired
survival in HIV disease. Proceedings of the National Academy of Sciences USA
(1997) 94(5):1967-1972.
[lix] De Simone, C, et al. High dose
L-carnitine improves immunologic and metabolic parameters
in AIDS patients. Immunopharmacol
Immunotoxicol (1993) 15(1):1-12.
L-carnitine improves immunologic and metabolic parameters
in AIDS patients. Immunopharmacol
Immunotoxicol (1993) 15(1):1-12.
[lx] Hellerstein, MK, et al. Effects of dietary
_n-3 fatty acid supplementation in men with weight loss associated with the
acquired immune deficiency syndrome: Relation to indices of cytokine
production. J AIDS Hum Retro (1996)11(3):258-270.
_n-3 fatty acid supplementation in men with weight loss associated with the
acquired immune deficiency syndrome: Relation to indices of cytokine
production. J AIDS Hum Retro (1996)11(3):258-270.
[lxi] Faure, P, et al. Vitamin E
improves the free radical defense system potential and insulin sensitivity of rats fed high fructose diets. _J Nutr (1997) 127(1):103-107.
improves the free radical defense system potential and insulin sensitivity of rats fed high fructose diets. _J Nutr (1997) 127(1):103-107.
[lxii] Basualdo, CG, et al. Vitamin A
(retinol) status of first nation adults with non-insulin-dependent diabetes mellitus. J Am Coll Nutr (1997) 16(1):39-45.
(retinol) status of first nation adults with non-insulin-dependent diabetes mellitus. J Am Coll Nutr (1997) 16(1):39-45.
[lxiii] Mak, RH, et al. The vitamin
D/parathyroid hormone axis in the pathogenesis of hypertension and insulin resistance in uremia. Miner Electrolyte Metab
(1992) 18(2-5):_156-159.
D/parathyroid hormone axis in the pathogenesis of hypertension and insulin resistance in uremia. Miner Electrolyte Metab
(1992) 18(2-5):_156-159.
[lxiv] Sanchez, M, et al. Oral calcium supplementation reduces intraplatelet free
calcium concentration and insulin resistance in essential hypertensive patients.
Hypertension (1997) 29(1 Pt
2):531-536.
calcium concentration and insulin resistance in essential hypertensive patients.
Hypertension (1997) 29(1 Pt
2):531-536.
[lxv] Facchini, F, et al. Relation
between dietary vitamin intake and resistance to insulin-mediated glucose disposal in
healthy volunteers. Am J Clin Nutr (1996) 63(6):946-949.
between dietary vitamin intake and resistance to insulin-mediated glucose disposal in
healthy volunteers. Am J Clin Nutr (1996) 63(6):946-949.
[lxvi] Nadler, JL, et al. Magnesium
deficiency produces insulin resistance and increased thromboxane
synthesis. Hypertension (1993) 21(6 Pt 2):1024-1029.
deficiency produces insulin resistance and increased thromboxane
synthesis. Hypertension (1993) 21(6 Pt 2):1024-1029.
[lxvii] Baum, M, et al. Inadequate dietary
intake and altered nutrition status in early HIV-1 infection. Nutrition (1994) 10(1):16-20.
intake and altered nutrition status in early HIV-1 infection. Nutrition (1994) 10(1):16-20.
[lxviii] Baum, MK, et al. Micronutrients
and HIV-1 disease progression. AIDS (1995) 9(9):1051-1056.
and HIV-1 disease progression. AIDS (1995) 9(9):1051-1056.
[lxix]
Reddi, A, et al. Biotin supplementation improves glucose and insulin tolerances in genetically diabetic KK mice.
Life Sci (1988) 42(13):1323-1330.
Reddi, A, et al. Biotin supplementation improves glucose and insulin tolerances in genetically diabetic KK mice.
Life Sci (1988) 42(13):1323-1330.
[lxx]
Koutsikos, D, et al. Oral glucose tolerance test after high-dose i.v. biotin administration in normoglucemic hemodialysis
patients. Ren Fail (1996)
18(1):131-137.
Koutsikos, D, et al. Oral glucose tolerance test after high-dose i.v. biotin administration in normoglucemic hemodialysis
patients. Ren Fail (1996)
18(1):131-137.
[lxxi] Koutsikos D, et al. Biotin for
diabetic peripheral neuropathy. Biomed Pharmacother (1990) 44(10):511-514.
diabetic peripheral neuropathy. Biomed Pharmacother (1990) 44(10):511-514.
[lxxii] Devara, JS, et al. The effects of
alpha tocopherol supplementation on monocyte function. Decreased lipid
oxidation interleukin 1 beta secretion and monocyte adhesion to endothelium. J Clin Invest (1996) 98(3):756-763.
alpha tocopherol supplementation on monocyte function. Decreased lipid
oxidation interleukin 1 beta secretion and monocyte adhesion to endothelium. J Clin Invest (1996) 98(3):756-763.
[lxxiii] Munoz, JA, et al. Effect of
vitamin C on lipoproteins in healthy adults. Ann Med Interne (Paris) (1994) 145(1):13-19.
vitamin C on lipoproteins in healthy adults. Ann Med Interne (Paris) (1994) 145(1):13-19.
[lxxiv] Peterson, JC, et al. Vitamins and
progression of atherosclerosis in hyperhomocysteinemia. Lancet (1998) Jan 24,
351(9098):263.
progression of atherosclerosis in hyperhomocysteinemia. Lancet (1998) Jan 24,
351(9098):263.
[lxxvi] Hickson, RC, et al. Glutamine
prevents down regulation of myosin heavy chain synthesis and muscle atrophy
from glucocorticoids. Am J Physiol [Endo Metab] (1995) 269(31):E730-E734.
prevents down regulation of myosin heavy chain synthesis and muscle atrophy
from glucocorticoids. Am J Physiol [Endo Metab] (1995) 269(31):E730-E734.
[lxxvii] Hong, RW, et al. Glutamine
preserves liver glutathione after lethal hepatic injury. Ann Surg (1992) 215(2):114-119.
preserves liver glutathione after lethal hepatic injury. Ann Surg (1992) 215(2):114-119.
[lxxviii] Opara, EC, et al. L-glutamine supplementation of a high fat diet reduces
body weight and attenuates hyperglycemia and hyperinsulinemia in C57BL/6J mice. J Nutr (1996) 126(1):273-279.
body weight and attenuates hyperglycemia and hyperinsulinemia in C57BL/6J mice. J Nutr (1996) 126(1):273-279.
[lxxix] Borel, MJ, et al. Parenteral
glutamine infusion alters insulin-mediated glucose metabolism.
J Parenter Enteral Nutr (1998) 22(5):280-285.
glutamine infusion alters insulin-mediated glucose metabolism.
J Parenter Enteral Nutr (1998) 22(5):280-285.
[lxxx]
Guthrie, R. Treatment of non-insulin-dependent diabetes mellitus with metformin. J Am Board Fam Pract
(1997) 10(3):213-221.
Guthrie, R. Treatment of non-insulin-dependent diabetes mellitus with metformin. J Am Board Fam Pract
(1997) 10(3):213-221.
[lxxxi] O’Neal, DN, et al. The effect of 3
months of recombinant human growth hormone (GH) therapy on insulin and glucose-mediated glucose disposal and
insulin secretion in GH-deficient adults: a minimal model analysis. J Clin
Endocrinol Metab (1994) 79(4):975-983.
months of recombinant human growth hormone (GH) therapy on insulin and glucose-mediated glucose disposal and
insulin secretion in GH-deficient adults: a minimal model analysis. J Clin
Endocrinol Metab (1994) 79(4):975-983.
[lxxxii]
Móldrup, A, et al. Multiple growth hormone-binding proteins are expressed on
insulin-producing cells. Mol Endocrinol (1989)
3(8):1173-1182.
Móldrup, A, et al. Multiple growth hormone-binding proteins are expressed on
insulin-producing cells. Mol Endocrinol (1989)
3(8):1173-1182.
[lxxxiii]
Gelato, MC, et al. Improved Insulin Sensitivity and Body Fat Distribution in
HIV-Infected Patients Treated With Rosiglitazone: A Pilot Study. JAIDS 2002;
31(2):163-170.
Gelato, MC, et al. Improved Insulin Sensitivity and Body Fat Distribution in
HIV-Infected Patients Treated With Rosiglitazone: A Pilot Study. JAIDS 2002;
31(2):163-170.